Welcome to the CATCH Study
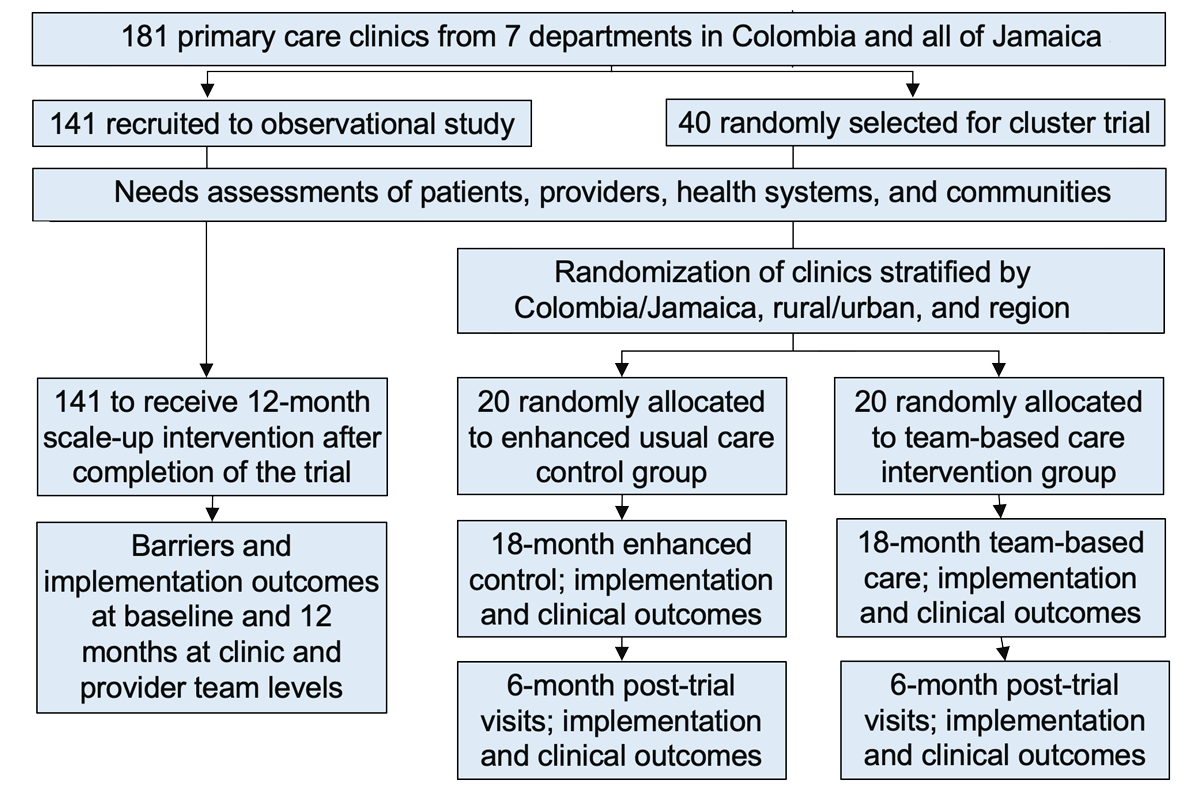
The overall objectives of the proposed study are to test the implementation and effectiveness outcomes of implementing and scaling up a team-based care strategy for hypertension control in Colombia and Jamaica.
Specific Aims
To test the reach, effectiveness, adoption, implementation (fidelity), and maintenance (sustainability) of implementing a team-based care strategy in primary care settings in Colombia and Jamaica.
To assess the barriers and implementation outcomes (acceptability, adoption, appropriateness, feasibility, fidelity, implementation costs, penetrance and sustainability) of scaling up a team-based care strategy in primary care clinics in Colombia and Jamaica.


A Collabrative Study
University of Santander (UDES) in Colombia
University of the West Indies in Jamaica
Tulane University in New Orleans, LA, USA
Phone
Study Design
Study Population
Eligibility criteria for clinics
- Serving >300 hypertensive patients during the previous year
- Clinic visits and BP medications are free of charge to patients
- Not sharing physicians, nurses, pharmacists, or CHWs with other clinics
Eligibility criteria for patients
- Men or women aged ≥21 years who receive primary care from participating clinics
- Average from 6 BP readings at two screening visits within applicable group:
- Untreated BP, no history of CKD, CVD, Diabetes: ≥140/90
- Untreated BP, history of CKD, CVD, Diabetes: ≥130/80
- Untreated BP, age ≥65: ≥130/80
- Treated BP: ≥130/80
- Not pregnant or planning to become pregnant in the next 12 months
- Able and willing to give informed consent
- No plans to change primary care clinic in the next 12 months
- Not an immediate family member of staff at the primary care clinic
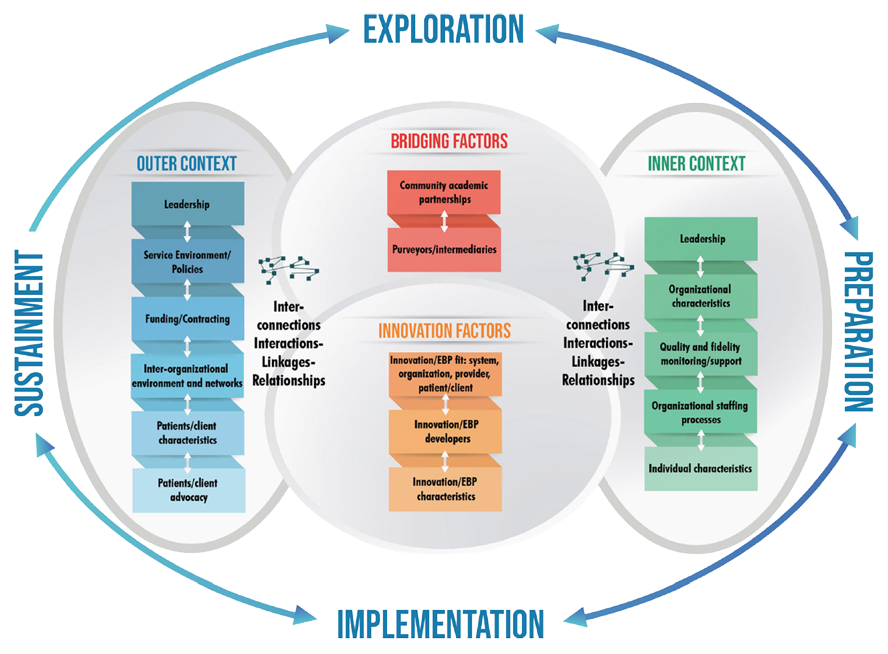
Implementation Strategies
Barriers to Hypertension and Strategies to Overcome Them
Intervention
The 2017 LASH hypertension guidelines with the treatment target of systolic BP <130 and diastolic BP<80 mmHg
Implementation strategy: team-based care
- Physicians will conduct a clinical evaluation of patients, choose initial BP medications based on a treatment protocol, approve medication changes based on patients’ responses, and supervise nurses and pharmacists.
- Nurses or pharmacists will meet with patients monthly to review clinic and home BP and to adjust BP medications according to a stepped-care treatment protocol.
- CHWs will function as case managers to coordinate patient care, regularly review patients’ clinic and home BP for feedback to the team, and coach patients on lifestyle changes and medication adherence.
- Patients will be empowered by home BP monitoring and lifestyle change.
- The team will meet monthly to review patient’s BP data and treatment plan.
RE-AIM Framework for Implementation
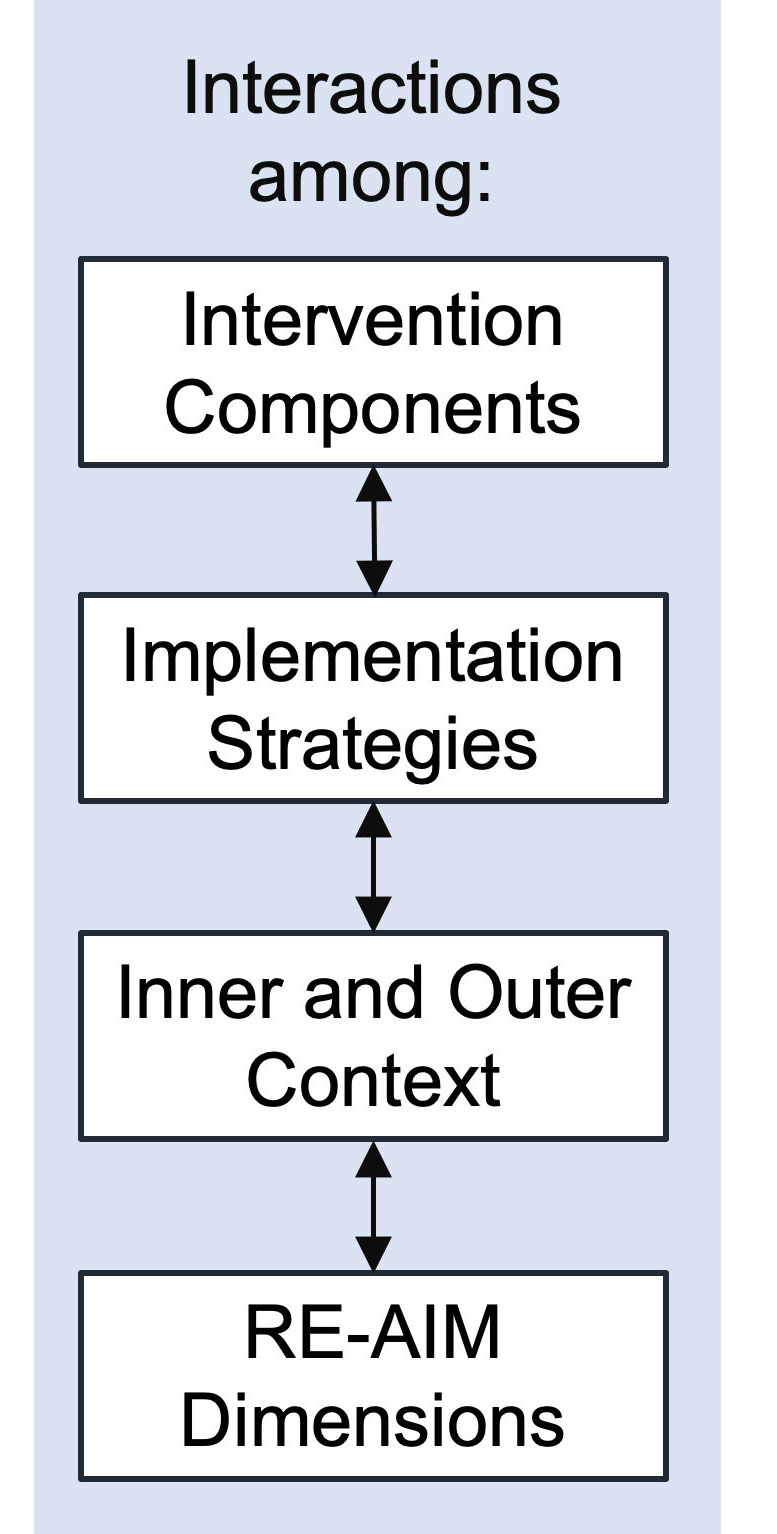

Implementation Outcomes
Implementation Outcomes • 1
Reach measures the proportion and representativeness of hypertensive patients who are willing to participate in team-based care.
- Reach will be assessed by the proportions of all eligible patients, all screened, and all contacted who are enrolled in the intervention clinics.
- Representativeness will be measured by demographic characteristics (e.g., age, sex, race/ethnicity, education, socioeconomic status, and health literacy) compared to regional and national data.
Penetrance measures the integration of team-based care within primary care clinics:
- the proportion of trained provider teams who are delivering team-based care;
- the proportion of trained nurses/pharmacists who are titrating medications;
- the proportion of trained CHWs who are conducting health coaching; and
- the proportion of enrolled patients who are receiving each component of team-based care.
Implementation Outcomes • 2
Adoption refers to the intention, initial decision, or action to utilize team-based care.
- Proportions of intervention clinics adopting team-based care and each component (i.e., protocol-based treatment, medication titration by nurse or pharmacist, health coaching, home BP monitoring, and audit and feedback); and
- Proportion of physicians, nurses/pharmacists, and CHWs attending training sessions.
Feasibility—the extent to which team-based care can be successfully used in intervention clinics will be assessed using survey and administrative data.
Acceptability (satisfaction) of team-based care will be surveyed in patients, physicians, nurses/pharmacists, and CHWs.
Implementation Outcomes • 3
Fidelity will be assessed at the participant, provider, nurse/pharmacist, and CHW levels.
- At the participant level, numbers and proportions of health coaching session attendance, home BP monitoring, and adherence to medication and provider visits will be measured;
- At the provider level, number and proportion of initiation or titration of medication according to clinical guidelines will be recorded;
- At the nurse/pharmacist level, number and proportion of medication titrations according to protocol will be documented;
- At the CHW level, numbers and proportions of health coaching sessions conducted, time and location of health coaching sessions, and numbers of clinic visit appointments made will be monitored.
Maintenance (sustainability): The extent to which team-based care is maintained will be evaluated at a post-trial follow-up six months after the end of the intervention:
- Proportion of intervention clinics maintaining team-based care;
- Proportion of trained physicians continuing team-based care; the proportion of trained nurses/pharmacists titrating medications;
- Proportion of enrolled patients continuing to receive team-based care; and
- Proportion of enrolled patients continuing home BP monitoring and BP control.
Clinical Effectiveness
Primary clinical outcome:
The difference in the proportion of patients with systolic BP <140 mmHg and diastolic BP <90 mmHg between intervention and control groups at 12 months
Secondary clinical outcome: the differences in mean changes of systolic and diastolic BP from baseline to 18 months between intervention and control groups
Additional effectiveness outcomes:
- side effects of medications
- change in quality of life measured by SF-36 score, and
- cost-effectiveness assessed as incremental direct costs (intervention and health care) per additional percentage of hypertension control

University of Santander
(UDES) in Colombia

University of the West Indies
in Jamaica

Tulane University
in New Orleans, LA, USA
Opportunities for Collaboration
We look forward to hearing about the other studies and are open to collaboration whenever possible.